November is Diabetes Awareness Month
As the diabetes epidemic surges across age groups, diabetic foot ulcers are also on the rise
November is Diabetes Awareness Month, a time to bring attention to this fast-growing, life-threatening epidemic. Currently more than 37 million Americans have diabetes and this number is expected to increase to 54.9 million by 2030. Increases have been attributed to a rise in obesity rates and an aging population, but new research shows that younger people are being diagnosed with the disease. From 2001 to 2017, the number of people under age 20 living with diabetes increased by 45 percent, and the number living with type 2 diabetes grew by 95 percent. This troubling development is expected to further challenge the healthcare system in the coming decades.
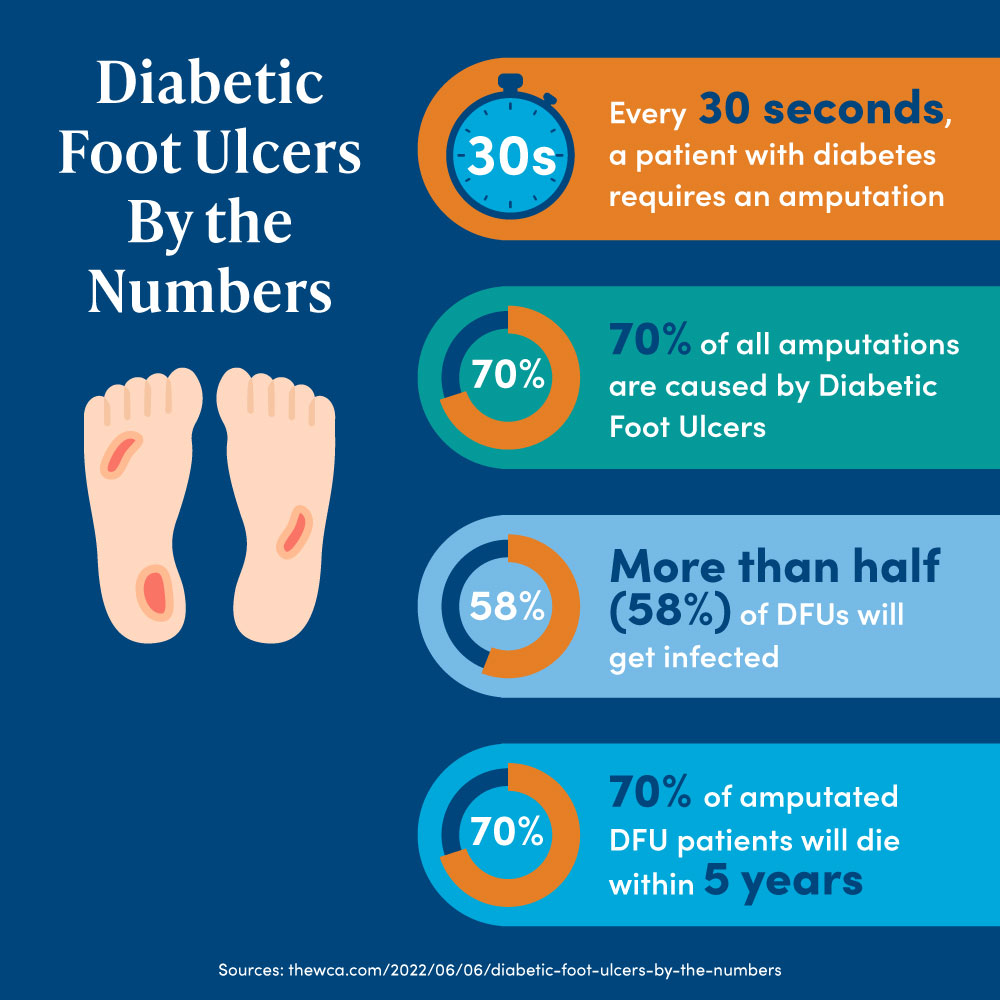
As the number of newly diagnosed diabetics increases, the incidence of complications including diabetic foot ulcers and related amputations is also on the rise. The COVID-19 pandemic has impacted young people with diabetes due to sudden and extended social isolation, sedentary lifestyles, treatment delays, and a general lack of consistency in disease management. Recent data reveals a 29 percent increase in diabetes-related deaths for younger people last year.
“Over the last decade we have seen a steady increase in younger people coming in with chronic wounds and diabetic foot ulcers, sometimes as young as their early 30s,” said Christina Le, CNO of Wound Care Advantage, a leading national consulting firm for outpatient wound care and hyperbaric medicine programs. “It is a disturbing trend and we are waiting for more data but it is definitely cause for concern.”
Diabetic Foot Ulcers: The Most Common Cause of Hospitalization Among Diabetics
The most common cause of hospitalization among diabetics is a diabetic foot ulcer (DFU), or an open sore on the lower limb that becomes infected. DFUs typically develop on weight-bearing areas of the foot, most commonly the bottom of the big toe, the ball of the foot or the heel. Approximately 15 to 25 percent of individuals with diabetes will be diagnosed with a DFU at some point in their lives, and one in five of these patients will undergo a lower limb amputation. In fact, every 20 seconds a diabetes-related amputation is performed. The five-year mortality rate is upwards of 74 percent for patients with lower extremity amputation - higher than those for several types of cancer including prostate, breast, and colon combined.
Why Are Diabetics More Vulnerable to Foot Ulcers and Chronic Wounds?
Uncontrolled blood sugar levels deprive the blood vessels of much-needed oxygen and nutrients, which are necessary for healing. To complicate things further, many individuals with diabetes have a loss of sensation in the lower limbs stemming from diabetic neuropathy. They may be unaware that a wound exists. On occasion, a trip to the ER for a high fever results in the discovery of a non-healing wound that has become infected. Many individuals with diabetes also have peripheral artery disease causing compromised blood flow to the feet, exacerbating the severity of the wound.
What Do People With Diabetes Need to Know?
A simple cut or scrape can quickly develop into a severely infected wound that does not heal and may be life-threatening. If a diabetic ulcer is suspected or discovered, a physician should be contacted immediately for an evaluation and possible referral to a wound care specialist. The general rule of thumb for most people is if a wound hasn’t healed on its own within 30 days, it should be evaluated. But if a patient has diabetes, early intervention is critical. With proper treatment, complications can be avoided.
“It’s important for people to know that a chronic wound in a diabetic patient can become infected quite quickly because of poor circulation,” said Dr. David Gustavison, Medical Director at Covenant Wound Healing & Hyperbaric Medicine Center. “If a patient gets evaluated early on, commits to treatment and is compliant with instructions, it will help prevent amputation.”
Wound Care Tips for Individuals with Diabetes:
- Check your feet on a regular basis, including the bottoms; contact a physician if a wound is discovered
- If you’re already in treatment for a chronic wound, keep all appointments and follow instructions
- To help promote healing, consume a nutritious diet with an appropriate mix of protein, fruits and vegetables, healthy fats and whole grains
- Limit alcohol consumption and avoid smoking. Smoking reduces circulation and impedes healing
At Covenant Wound Healing & Hyperbaric Medicine Center we’re using advanced wound care modalities to quickly and successfully treat non-healing wounds. Chronic wounds can be diagnosed, effectively managed and ultimately healed, oftentimes within eight weeks. Contact us at 989.583.4401 for more information.
Posted Date: 11/1/2022